Advocates are working to get the same services covered for trans men and women that are covered for everyone else.
 Jay Maddock has known he was a man for most of his life, even though that’s not the body he was born with. At age five, he told his dad he wanted to be a man, and was fortunate to grow up in a family that didn’t push gender stereotypes.
Jay Maddock has known he was a man for most of his life, even though that’s not the body he was born with. At age five, he told his dad he wanted to be a man, and was fortunate to grow up in a family that didn’t push gender stereotypes.
After spending 10 years living as a gay woman, Maddock decided he wasn’t going to let another year go by without living his real life. At age 25, he came out as a transgender man, and in 2011 he began his medical transition with therapy, testosterone injections and surgery to remove his breasts.
“I’m so lucky that my family has loved me from day one,” says Maddock, who is executive director at Michigan’s Kalamazoo Gay and Lesbian Resource Center. “So many people in the trans community don’t have the support I have always had.”
In fact, friends helped him pay for his surgery, which was not covered by his insurance — even though Blue Cross Blue Shield of Michigan, his insurer, would cover reconstructive surgery for a woman with breast cancer after a mastectomy.
They understand that breasts are a sign of femininity but they didn’t understand that a trans man would want to be rid of that femininity. After my voice changed they always called me ‘sir’ but weren’t able to get me any coverage for my surgery.
Insurance exclusions like these are an ongoing problem for the transgender community, even though most major medical societies, such as the American Medical Association and the American Psychological Association, recognize gender reassignment surgery and other transition care as appropriate for people suffering from gender dysphoria, which is a sense of “incongruence” with the sex they were assigned at birth.
Even the U.S. Department of Health and Human Services (HHS) has lifted a 33-year-old ban on Medicare coverage for gender reassignment surgery, recognizing it as a medically necessary step for some transgender people.
But not every insurance company has caught up. And others, like Blue Cross Blue Shield of Michigan, are actually taking away coverage they used to provide.
Maddock received a letter from the insurer earlier this year, telling him that transgender procedures or related medical care would not be covered under his plan anymore.
He’s about to run out of the testosterone he takes to keep his hormone levels consistent — something his doctor told him was extremely important for his health. So Maddock will have to pay more than $100 every six weeks while he fights to get his medication covered again.
This is a medical necessity. Regardless of your stance on trans people, you’re talking about a human being. My body has become accustomed to receiving testosterone. You’d never cut someone off cold turkey if they were on hormones for another reason. That’s dangerous.
Understanding the healthcare needs of transgender people.
According to Amy Hunter, an LGBT activist, stopping hormone therapy suddenly does have health risks. The use of hormones themselves has risks — something transgender people and others, such as women with breast cancer, accept as having benefits that outweigh those risks.
“If insurers are aware you’re transgender, they are sometimes denying ancillary care for risks of hormone use, such as heart problems and breast cancer in trans women,” says Hunter, a fully transitioned woman. “It endangers people’s lives and puts a financial hardship on a community with one of the lowest median incomes in the country.”
There’s another critical aspect to all this, which is the emotional well-being of trans people, who have higher rates of suicide, anxiety, depression and self-abuse, says Andrew Cray, a policy analyst for the LGBT Research and Communications Project at the Center for American Progress in Washington, D.C.
“There’s well-documented evidence that for trans people, their identity is very tightly bound up in gender dysphoria before they begin medical aspects of gender transition,” he explains. “They struggle because of a mismatch between their gender identity and the gender they were born with.”
Both Hunter and Maddock describe the painful period before they began transitioning as a time of feeling very disconnected from themselves.
 Maddock struggled with depression beginning in puberty, performing self-mutilation and contemplating suicide. Fortunately, his mom put him in therapy, even before Maddock really understood why he felt so different.
Maddock struggled with depression beginning in puberty, performing self-mutilation and contemplating suicide. Fortunately, his mom put him in therapy, even before Maddock really understood why he felt so different.
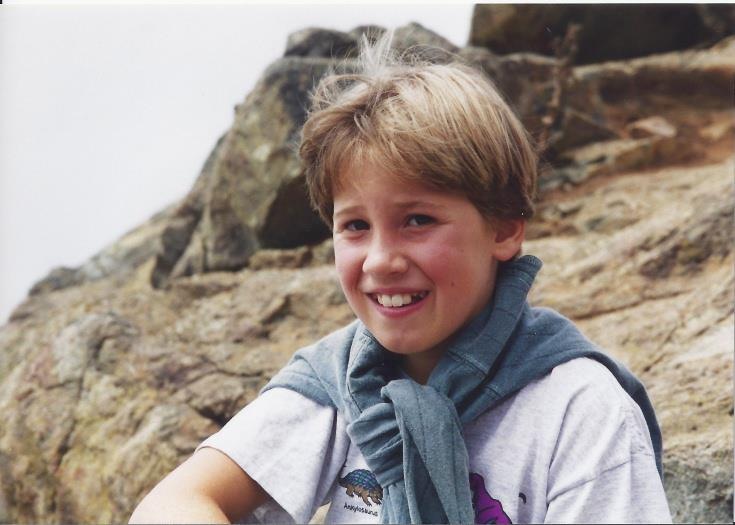
But he does have what he calls “lost boy” memories — fleeting glimpses of knowing he was really a boy and not a girl. He remembers two photos taken the same day in his childhood that tell the story.
My grandma used to buy me frilly dresses and I would cry. In one photo I’m wearing a dress and am glaring jealously at my brother, who is wearing jeans. In the second photo, I’m wearing pants with a leather jacket and grinning ear to ear.
Hunter and Maddock can both attest to the joy that comes from living the life they were always meant to, which underscores the medical necessity of transition surgery. It’s important to note that not every trans person chooses surgery. Many find peace of mind from hormone therapy, electrolysis, voice therapy and other non-surgical approaches.
Eliminating discrimination by health insurers.
Michigan Consumers for Healthcare (MCH) is one of the organizations working to make sure coverage is provided to transgender people in exactly the same way it’s provided to everyone else.
“MCH is looking at this issue like we do every issue: All consumers deserve the coverage they need and that they and their medical providers deem appropriate,” says Ryan Sullivan, policy director at MCH. “That means making sure they have access to the services that will improve their health.”
In choosing plans that would be offered under the Affordable Care Act (ACA), many states — including Michigan — did not include any plans that include coverage for transgender people.
Some insurers have claimed that all they have to do under the ACA is provide the ACA’s “10 essential health benefits” such as routine screenings and annual check-ups. But, as Sullivan points out, those essential benefits are the bare minimum — and specifically excluding a particular community from coverage access is discriminatory.
“There’s a lot of pretty pointed language coming out of Washington, D.C., that says you can’t treat transgender individuals in a discriminatory fashion,” says Sullivan. “We think it’s the state’s role to ensure equal, non-discriminatory coverage to people within the spirit and the letter of the ACA, and HHS has been pretty clear about that.”
MCH and other advocates are hoping to work collaboratively with the Michigan Department of Insurance and Financial Services (DIFS) and Michigan’s insurance providers to design plans that include coverage for transgender people.
Cray emphasizes that in other states where insurers have extended coverage to transgender people for complete transgender transition, such as Massachusetts, it involves little or no increase in cost to the insurers or other customers. And it’s simply the right thing to do.
The majority of places that have examined cost evidence have found extremely low utilization — there’s not a sudden influx of transgender people flocking on a plan. When spread across the entirety of an insurance pool, the costs are extraordinarily low. They’re often zero, and have no material impact on premiums.This is medically necessary care that’s covered for others. Hormones, for example, are part of the care for many people, such as women coping with menopause or people with various endocrine disorders. They’re also part of treatment for trans people. Transgender people are in our communities — they’re our friends and neighbors, and this is care they need to lead healthy, authentic lives.
Sullivan underscores the fact that MCH and other advocates aren’t asking for any special treatment for transgender people. They’re simply asking for the same access to coverage that everyone else receives.
You can’t exclude people from treatment for their medical needs just because you’re uncomfortable with who they are. This is a consumer issue that touches on basic concerns we have for all consumers. We don’t see this as a special population. We’re all up against danger when insurers design plans around conditions that are difficult to treat or misunderstood. We can’t let insurers use existing ignorance and discriminatory attitudes to design coverage.
The ACA did away with a lot of discrimination in the insurance industry, but there’s much more work to be done. Stay tuned for updates on this issue as Michigan advocates continue working to ensure that no one is discriminated against by insurance companies, for any reason.
Want a more in-depth understanding of transgender health issues? Watch this terrific TEDMED Great Challenges discussion featuring a team of experts.
[Photos courtesy of Jay Maddock]